A sombre, six-sentence paragraph was the final communication that Dr Fred Muoki penned before he died. It was not a will, but a suicide note addressed to his sister. He was sorry that the pressures of life had knocked him down.
He was a rising star that many expected to shine bright; a hardworking young man whose hopes for a better life were dimmed by a society and government that neglected him, and many like him.
“I’m sorry sister. I have a lot of pressure. Debts and loans from my friends. I am sorry to disappoint you. I don’t have money in my account so don’t bother checking. I am deeply sorry sister,” he signed off, before taking his own life.
Muoki is said to have struggled for months to get a job after graduating from medical school, but all attempts hit a snag.
A dark cloud hung over him. The pressure from society sent him to the pits, where he had no strength left to fight.
He needed to provide for his loved ones, but with what income? He needed to live his dream of restoring people’s lives, but who was to give him that chance? He needed to earn his doctor title, but it remained just a name, his skills underutilised.
Muoki, unfortunately, is just one among an increasing number of Kenyan doctors who are taking the dark route to the abyss, after seeing their hopes for saving lives, and a rewarding career, dashed.

According to data by the Kenya Medical Practitioners and Dentists Council, about seven medical doctors in the country have died by suicide in the past seven years after they failed to get an opportunity to practise medicine.
After a grueling six years in medical school, doctors usually look forward to saving lives –but those coming out of school these days wait longer than usual.
About 4,000 trained doctors in the country are jobless, despite both public and private hospitals being overwhelmed by few staff dealing with thousands of patients who turn up for treatment on a daily basis.
In whose hands are the patients safe, one would wonder, for those at work are burnt out, compromising the quality of their output, while others stay at home in frustration, on the verge of slipping into depression?
More than 5,000 doctors have graduated in the past five years, registered and licensed to practise by the Kenya Medical Practitioners and Dentists Council.
Of these, about 3,800 are medical officers, 272 dentists and 1,280 pharmacists.
Last year had the most doctors getting registered; 1,330. The year 2020 had 1,321 doctors joining the market, 2018 (979), 2021 (955) and 767 joined the profession in 2019.
Out of those 5,352 registered in that period, only 1,000 doctors have been employed, with the rest joining the growing list of unemployed graduates in the country.
Nairobi County employed the highest number of medical practitioners in the last five years, having absorbed 134 followed by Kisumu and Kitui employing 58 medical practitioners each.
Mombasa (45), Murang’a (44), Lamu (36), Machakos (34), with Kiambu, Mandera and Laikipia employing 33 medical practitioners each.
The KMPDU data shows that in the past five years, Uasin Gishu County has employed only two medical doctors, while Kajiado, Samburu and Elgeyo Marakwet have hired three each.
Baringo has four, Narok five, Bungoma six, Kisii seven, with Nyamira employing eight doctors in the past five years.
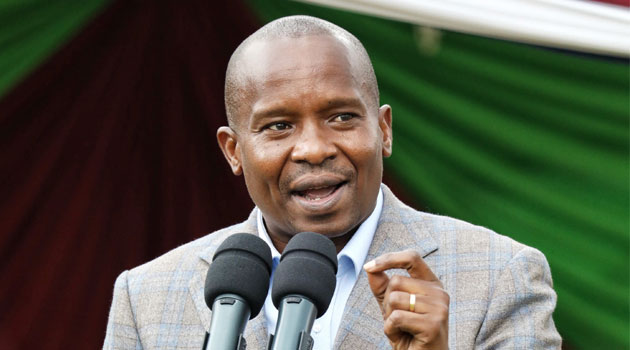
The Union Secretary General, Dr Davji Atellah, told Saturday Nation that only about 20 per cent of the medical practitioners that have graduated have been employed since 2018.
Despite health being a devolved function, counties do not employ doctors on a yearly basis as the national government would do before advent of devolution, deepening the doctor joblessness crisis.
“This is why we have many hospitals in the country with minimal doctors hence not many can give quality healthcare to Kenyans,” Dr Atellah said.
Before 2017, every doctor being churned out of university post-internship got employed, as the Health ministry at the time would post them to different hospitals across the country.

“This stopped and employment stopped as well. That’s why there is a long waiting-list of Kenyans waiting for procedures to be done. Even specialists are left out. For instance, there are many cases of cancer that go undiagnosed because of the shortage of specialists,” he said.
“If we have the doctors employed then the burden will be reduced. The only way we can have functional and access to healthcare as described in the Universal Health Coverage is to have doctors employed,” he added.
In Africa, according to Dr Atellah, Kenya is the only country that has a surplus of unemployed doctors and a biting shortage in the hospitals.
“I really feel for my colleagues who, after spending six to seven years doing a course, they still have to toil for years looking for employment or work under precarious contracts that don’t offer them similar benefits as their older colleagues,” Dr Atellah said.
“For those lucky to be employed, they work long hours, with no leave days, no medical cover, no study leaves and inferior pay with illegal clauses in their contracts barring them from joining the union or participating in union activities. When these inhuman contracts run out, they don’t get renewed and neither do they get their gratuities paid,” he added.
The Union has since called upon the counties to close the gap between the number of graduates and the shortage being recorded in the facilities so that skills are not wasted and hospitals hire as many fresh recruits as they can to help tackle the widespread shortage of medics.
With many waiting to be hired, the few employed ones are struggling to attend to millions of Kenyans crowding the functional facilities.
Multiple interviews by the Sunday Nation has revealed that most of the unemployed doctors have now ventured into business, some unrelated to their profession, while others are doing part-time shifts in private facilities, earning their pay for the hours that they render their services.
Dr Atellah said that doctors who stay for too long without finding employment usually contend with low-paying jobs at private hospitals to fend for themselves and their families.
It takes seven years to train as a medical doctor, including a year of compulsory internship. The cost of training one medical doctor ranges between Sh4 million to Sh5 million.
“It’s sad that a nation would spend so much on training its greatest brains in one of the noblest professions and fail to utilize them to save the lives of Kenyans who continue to die from treatable illnesses,” said Dr Atellah.
There are more than nine universities in Kenya currently offering medical training.
Others obtain medical education from international universities and return home to contribute to the country’s healthcare system.
“It is sad to note that for past six years, Kenya seems to have adopted a policy of train and dump,” he said.
They now want the government to put in place measures to have annual recruitment of doctors, just like it is done for the military, police officers and teachers; until the country achieves the World Health Organisation (WHO) recommended doctor to patients ratio of 1:1,000.
We are currently at 1:17,000. “This is unacceptable,” he said.
According to WHO, the prescribed health worker to patient ratio is determined as 23 doctors, nurses and midwives for every 10,000 people.
However, data shows that the health workforce ratio in Kenya currently stands at 13 doctors, nurses, and midwives for every 10,000 people.
They also want the management of human resources for healthcare to be centralised and standardised to reduce the many industrial actions that are occasioned by disputes with the county governments.
“The Health ministry announced that the plan to hire 20,000 healthcare workers to bridge the doctor, nurse and midwife ratio recommended by WHO is in the pipeline, but how long is this pipeline?”
Health Cabinet Secretary Susan Nakhumicha in an interview with Nation said that health workers will be recruited over a three-year period subject to the availability of the Sh21 billion that is required by the ministry to bring them on board.
Nation